Managing a clinical service
I had a recent, unexpected change in my role and have been reflecting on what I have learned and which parts of it might be useful to share. This has given me insight into the tremendous work behind the scenes in the NHS. Thankfully, both my colleagues are now healthy and back at work.
A sudden change
Our clinical director tested positive for covid19 and although he is an extremely healthy and fit person, he got really sick, really quickly. At the same time, one of my other consultant colleagues also became seriously unwell with a non-covid illness. We are a team of 9 whole time equivalents and over the course of about 24 hours, we were suddenly down 2 whole time consultants. The first reaction of everyone was shock and of course, tremendous concern for our colleagues. We felt powerless to help. The unit was going through a particularly busy patch of clinical work and we had big holes in the rota. I think sometimes people think consultants are invincible and all –knowing but believe me we are not! We are human, we get scared and sometimes we don’t know what to do for the best. However, we are good at teamwork and coming together to solve problems. The collective decision (we were able to include our CD in this) was that I would take on the clinical director role- with the rest of the team supporting.
What does a clinical director do?
This is something of which I had very little knowledge as a junior doctor and even as a consultant, was relatively naïve about. I was in a fortunate position though, as the service was in good shape and structures were in place which meant that many things could continue to tick over whilst I was scratching my head trying to figure out the basics.
Who’s who
One significant basic was working out who is who in the organisation. This is essential a. to get anything done and b. not to look like a plonker at various meetings.
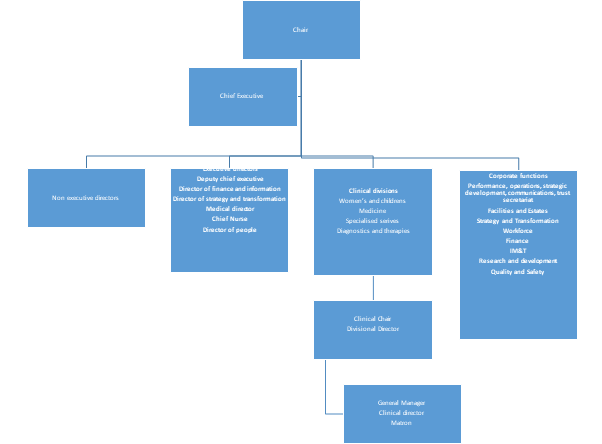
As a front line clinician I had little knowledge of the roles, let alone the names and faces of the highly skilled, engaged and passionate people who work in non-clinical roles in our trust. As a trainee I had even less understanding of how the hospital is managed, lines of accountability and how money flows through the organisation. However, better awareness of the workings of a department and organisation would help trainees to effect change in the NHS. Many trainees have great ideas – they work at the coal face of the organisation- they can see the problems and the obstacles but they often don’t know how to get a project off the ground. During my time as acting CD I got to know more about our management team. Their role and working practices are not dissimilar to mine- they also work long hours (often leaving the building later than me) and are on call out of hours as well. Our manager and I met to deal with a varied range of problems from leaky pipes, complaints and rota gaps.
How is our service funded?
Neonatal Medicine is a part of the NHS which is specially commissioned. This means that our funding comes from close to the source of the funding stream for the NHS and not downstream via the clinical commissioning groups.
https://www.kingsfund.org.uk/audio-video/how-is-nhs-structured-funding-flow
A group of experts in the field decide how this money is best spent- they are the Clinical Reference Group. Service specifications set out what each type of unit or service is expected to deliver.
https://www.england.nhs.uk/commissioning/spec-services/npc-crg/group-e/e08/
Each neonatal service will collect data to track how it is performing according to the service specifications. For example, each month we receive data on how many babies required intensive, high dependency or special care that month and track this over time which also enables planning for the future.
Inbox overload
Pretty much as soon as I took over the role, my inbox filled. It would crash about twice a day, even after I had requested an expansion! I cannot pretend that I found the solution to this. There are probably lots of brilliant hacks which I haven’t discovered for how to organise email traffic efficiently. My strategy involved trying to check regularly and prioritise. I sent emails acknowledging that I had received the message and asking the sender to prompt me if they didn’t get a response within a particular time frame. With our team we have agreed to set an achievable time frame for when we require responses- eg within a 2 week period- and we send reminders. I tried to ensure my out of office replies and e signature were current. This is definitely an area where I still have lots to learn but I at least now have a better understanding of the volume of emails that anyone in a leadership role has to deal with and will have a more compassionate response when a person might not reply or be slow to do so.
Backup
I was in a new role with no induction and no training. The great thing was I had loads of help – I just needed to ask for it. We ensured as a team we interacted regularly- weekly consultant meetings with good attendance were achieved with video calls and we used WhatsApp in between. We have some rules of engagement around these to protect time off whilst hopefully providing good, rapid support to the team- especially those on clinical service. One of the brilliant things my team did was immediately to offer to share out some of my other workload- various projects and meetings were taken off my hands which was a huge help. Another fantastic source of backup was the matron and nursing senior leadership team, without whom I would have been utterly at sea.
Meetings
There are a lot of meetings in the NHS! I remember my brother, who is also an NHS consultant, telling me he once went to a meeting about going to meetings! My first challenge was finding out which meetings there were and then which I was expected to attend and after that which ones it was useful for me to attend! Chairing meetings is also something of which I had minimal experience. My tip for this is taking time to prepare. Write an agenda and follow it to structure the meeting and keep it running to time. Find out who everyone is on the attendance list and their role- I used the hospital connect email system to look at role titles and then occasionally Google, when I didn’t know what a role meant. Being new does bring a huge advantage because people don’t expect you to know a great deal and so I could ask daft questions about how systems worked and what roles everyone had (and to be honest, I occasionally got the feeling that others in the meeting were pleased I had asked those things as well).
Workforce
There were huge pressures on the medical rota, as I’m sure most departments have experienced in the pandemic. Our department has a meeting first thing Monday morning to look at all the rotas for the coming week- this is essential to plan for unexpected absences. One of my wonderful colleagues manages our “locum army” who are an amazing group of junior medical staff who will cover short notice rota gaps for us. I have to say we really do feel like they are an invisible back up force who will swing into action when we call- thank you so much guys. Recruitment and retention is a significant area and another colleague does a tremendous behind the scenes role preparing job adverts and then short listing (we are very fortunate to get many applicants). Running interviews on line has become the norm and I think we are providing a pretty good and efficient experience for people with this.
Care & Self Care
Having an open door is an important part of the clinical lead role. It is a huge privilege to work with a large and wonderful group of people. From time to time, all of us will have additional pressures from outside work, which will inevitably impact upon us and sometimes our capacity to work in our usual way. I realised that being a clinical leader also means caring for the team, listening and being flexible to help in whatever practical way possible. Self-care is an essential component of this. As they say, you need to fit your own oxygen mask before helping others.
Management Experience for Trainees
I asked a couple of colleagues in management if there was anything they would wish trainees to know about their role. They both said that they are very much part of the team and there to assist where needed- from anything from problems in the here and now to securing funding for the service for the future. Always feel free to approach them with any issues. Their role is to enable services to run smoothly and develop over time, not to block or obstruct changes. Trainees might want to spend a day shadowing a manager (I did this when I was training and it was very helpful) and also to sit in on some departmental meetings- ask your clinical directors about this.
So now I’m back in my usual role as a NICU consultant and subspecialty tutor. I’ve learned so much- about the service, the team and about myself which was a tremendous privilege and I’m so thankful that my colleagues are back at work and healthy again.

Wonderful post, Beth! Thank you for sharing and for being so open and honest about your experience. I’m really glad everyone is doing better 🙂
LikeLike
Fabulous blog Elizabeth – loved reading it & I am sure you did a fab job 👏 It also brought back memories of when I stepped up to become NICU CD in 2013, first nurse in UK to take on this role. Steep learning curve & lots of googling…I was in post for 6 years. My legacy is that I teach/lecture MSc nurses & trainee doctors on the NHS structure -‘Parliament to the cot’ – & try to make sense of it for them. I stress that although clinical shop floor work is hugely important, without the infrastructure behind it, governance, education, management, charity etc etc the service wouldn’t function & encourage them to ‘be kind’ & acknowledge their colleagues in that role.
LikeLike